Criteria for open platform in AHA and AAL domains which vCare complies with:
Open Source
Open Standards Based
Shared Common Information Model
Federatable
Vendor Technology Neutral
Supports Open Data
Open APIs
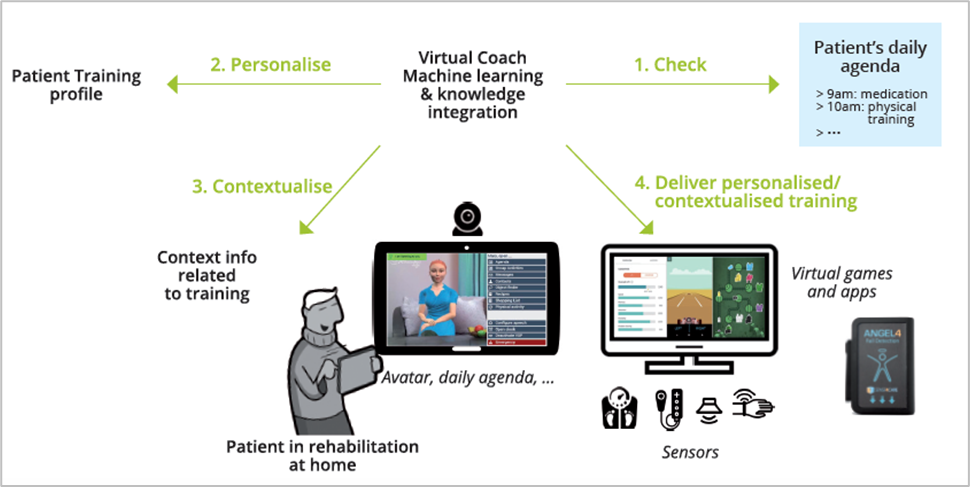
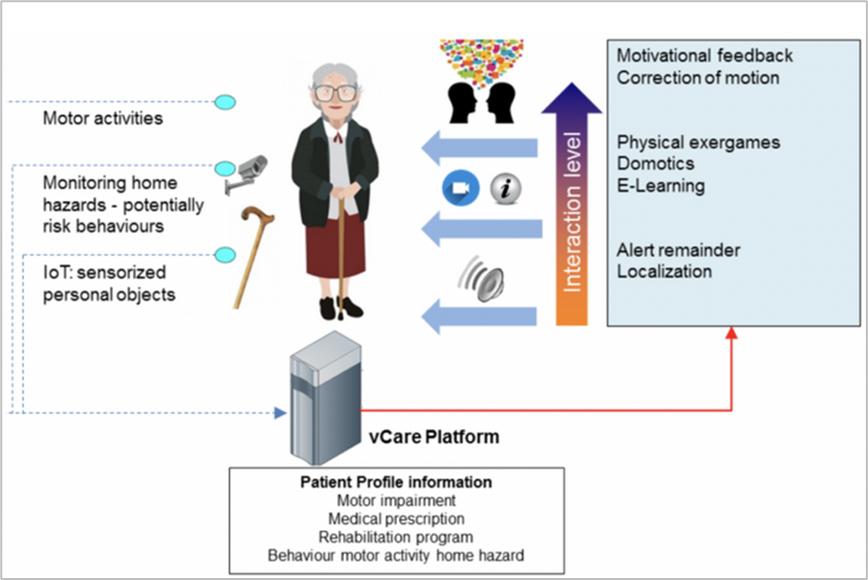
Secondary prevention is an essential element of long-term rehabilitation. To improve this situation, strategies oriented towards risk reduction, treatment adherence, and the optimisation of quality of life are need to be developed. The vCare virtual coach supplements the usual rehabilitation processes and adopts strategies that empower the patient and his/her caregiver. The personalised rehabilitation clinical pathway is activated by the clinician interaction with the patient on the basis of evidence-based expert rules. It also evolves constantly in function of the patient choices and the rehabilitation goals. Adaptation of the clinical pathways is ensured by embedded machine learning engines and the integration with contextual and medical information provided by sensors. The data are processed continuously to provide appropriate advice and feedback to the patient.
The clinical staff can monitor the evolution of the patient’s situation at any time. There is a wide range of interactions with the virtual coach available through the avatar displayed on the tablet. These interactions include arranging the best time schedule for the rehabilitation sessions, offering precisions and feedback about the exercises, and advising the patient about good practices to enhance his or her well-being. While the avatar can promote activities which trigger social interaction and ‘virtuous’ behaviors, it can also alert the patient when his/her behavior is inappropriate (e.g., whenever the behavior is too risky or the person is insufficiently active). vCare services can be used by patients with very different conditions, which include strokes, cardiovascular conditions like ischemic heart disease and heart failure, and neurogenerative conditions like Parkinson’s.
Need more info? See more partners here.
IT aspects of vCare
vCare integrates in a virtual coach system a set of solutions developed by four members:
By integrating these technologies in a single platform, the virtual coach of vCare provides the patient with a number of services clustered into:
The major advance of vCare is an adaptive integration and use of services according to a personalized pathway. To achieve this, semantic technologies are used to allow service (re-)configuration. The semantic shell is developed based on an ontology that contains information about the patient’s needs and conditions, services, context information and pathways.
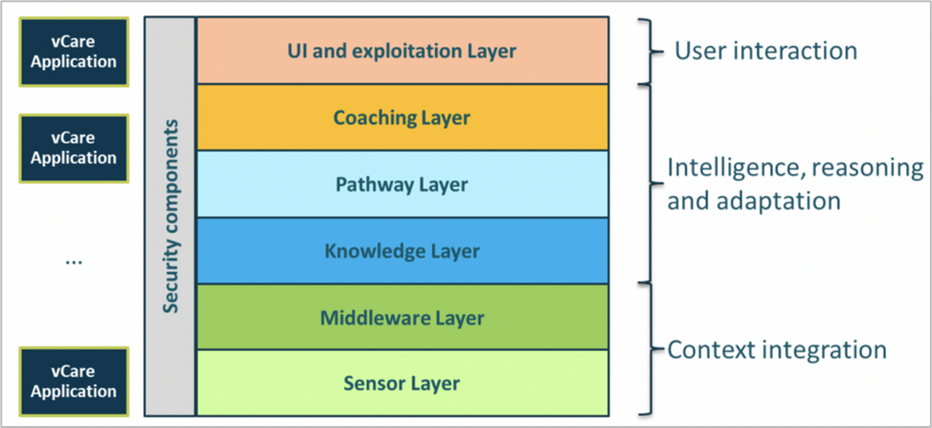
The vCare system is described as a “stack”. It comprises six layers, which are assigned to three groups (i) context integration, (ii) intelligence, reasoning and adaptation, and (iii) user interaction (the graphic shows these from the base/context through to the highest level of the interaction with the user/patient).
The context integration group is composed of the sensor and middleware layers of software. They are responsible for integrating both smart home context data and health monitoring devices. They build on established technologies such as FIWARE (a curated framework of open-source platform components to accelerate the development of Smart Solutions). The sensor layer is responsible for integrating contextual information from the environment as well as health monitoring information from the patient. Both are gathered at the home of the patient. The middleware layer then provides both cloud storage capabilities and semantic integration for the information coming from the sensor layer.
Intelligence, reasoning and adaptation are at the core of the vCare system. The pathway layer offers clinical pathway templates for various rehabilitation services, provided by the coaching layer. The vCare coaching services are very varied. They include physical and cognitive training, e-learning, and rehabilitation coaching for therapy assistance. The knowledge layer personalises pathway templates on a patient level and provides intelligence and reasoning capacities to adapt these pathways as the patient’s treatment progresses. Here, the vCare ontology models the semantic structure of the available data in order to integrate it with external knowledge bases and datasets.
The user interaction layer, consisting of the user interface (UI) and exploitation layer, integrates various interaction devices and provides access to external third-party applications and services. The layer is responsible for interaction with the patient. It enables speech input and speech synthesis as well as providing textual input to communicate with the vCare avatar.
The complete vCare system stack of software applications is protected by security components providing identification, authentication and authorization.
vCare rehabilitation applications are developed by using all resources provided by the full vCare system stack.
For a more detailed description of the vCare project architecture and services, please read the vCare white paper.
Technology Readiness Level (TRL)
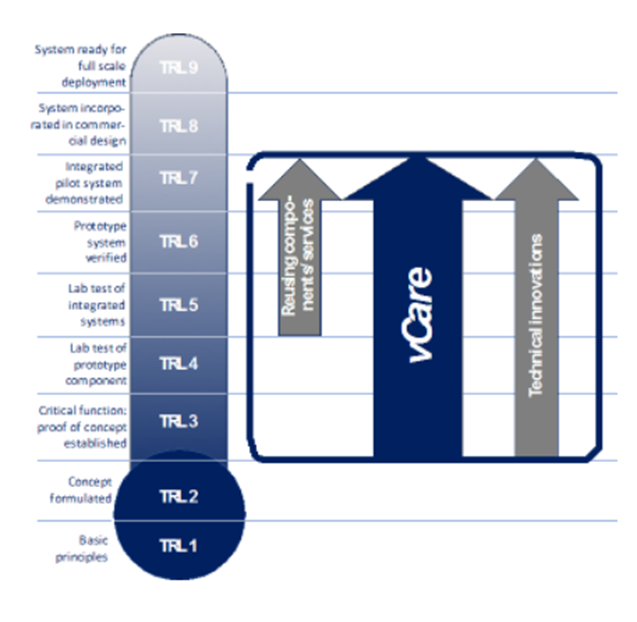
The project’s approach requires a distinctive view on the technology readiness levels (TRLs).
Since the project focuses on integrating existing technologies rather than implementing another single, monolithic solution, the components used are based on a lab test of integrated systems (TRL 5). Further technical innovations will be developed during the process, based on technical concepts and proof of concept implementations (TRL 3). As vCare aims to conduct a small-scale pilot, the project will advance the virtual coaching solutions from the level of a proof of concept (TRL 3) to an integrated and demonstrated pilot system (TRL 7).
Living with a virtual coach
This story illustrates the impact of a virtual coach on the daily life of older people. It uses the example of an older lady living in Milan, Maria, who has had a stroke and is now back living in her home environment.
This deficit causes functional motor impairment and Maria has serious problems in managing her life both in domestic environments and in open spaces. The physiatrist prescribes an eight weeks long session of motor rehabilitation treatment using serious games. In addition, the physiatrist suggests light motor activities during the day, the use of an aid (walker/cane) whenever she walks and, to reduce the risk of falling, the avoidance of complex tasks, such as picking up an object fallen on the floor, while remaining in standing position. Back home after being discharged from hospital, Maria needs to gradually learn how to relate to her virtual coach (under the form of a human avatar), which constantly supports her in both her motor and cognitive rehabilitation.
But motor and cognitive rehabilitation is only part of the story. The customized care plan offered by the coach includes also home risk prevention tips, social and well-being promotion, emotional support, practical video tutorials, and physical activity monitoring, to name a few. These features are triggered by specific events and are constantly adapted to Maria’s situation and actions.
The virtual coach is also meant to support Maria’s psychological state and to encourage behavioral change in order to support Maria’s adherence to the care and rehabilitation plan established by her healthcare provider.
The virtual coach encourages Maria to remain active. It monitors periods of inactivity and continuously stimulates Maria by e.g. proposing a short walk outside if the weather conditions are good. As a result, she will progressively regain a better quality of life, with a progressive reduction of the pain and fatigue that she experienced after her stroke.
There are thousands of health-related thoughts in Maria’s mind that, sometimes, she feels uncomfortable telling anyone: she is afraid of not being understood, repeating the same questions, or is embarrassed to disclose (even to people who could help her). Maria’s weekly experience is scattered with worries and fears about her recurring problems, related to pain in her shoulder, lack of dexterity in her right hand, and disturbance in her gait. Maria complains about difficulties in using her right hand and often says “I feel maladroit and useless”, “I am disappointed about not being able to cook like before”. But surprisingly, Maria’s beliefs might however change over time. Step-by-step, through daily interactions, the virtual coach will help Maria to find the right answers and regain self-confidence.
Thanks to her virtual coach, Maria has now the best chance to complete her rehabilitation in an optimal way.
vCare to help answering crucial needs in Romania
Cardiovascular mortality is a critical public health problem in Romania. It is three times higher than in any other state of the European Union. With a reduced average life expectancy of 8 years in men and 5 years in women compared with the European figures, the prevention of cardiovascular disease is currently one of the top priorities of the Romanian Ministry of Health. The main causes of hospitalisation among cardiovascular patients are heart failure and ischaemic heart disease with an annual incidence of 4.7% and 5-7% respectively of the country’s population.
Romania: Cardiovascular disease takes the largest toll on mortality but cancer deaths are increasing
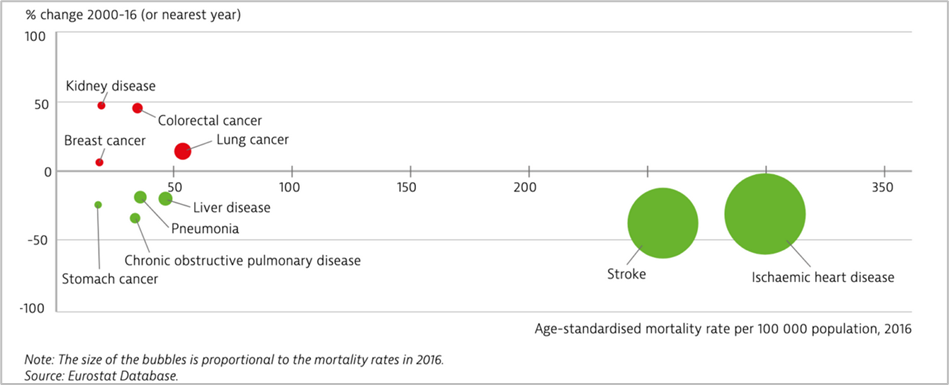
Stroke and ischaemic heart disease remain the main causes of mortality in Romania. Cardiac rehabilitation is now recommended to every eligible patient diagnosed with heart failure and ischemic heart disease in the country. However, the absence of free-of-charge ambulatory rehabilitation puts Romania in the last place in Europe in the management of secondary prevention of these life-threatening pathologies.
Romania focuses on testing the technologies in a living lab
vCare project aims to build, through machine learning, software which will allow patients to perform cardiac rehabilitation in the comfort of their own homes. We are now at the step of working in a living lab. The testing of the integrated system is taking place at the Bagdasar-Arseni Emergency Clinical Hospital in Bucharest, where the vCare team has created all the conditions necessary for the optimal development of the project. In a bright and spacious room, we have put together three zones: an exercise area (consisting of 2 cycloergometers[1], a smart TV, and sensors), a relaxing corner (with a couch, coffee table, hallstand, and mini-fridge), and a fully equipped bathroom.
The project consortiun conducted an assessment to evaluate users’ perceptions of the integration of the solution in their daily lives. Preliminary analysis in the living lab highlights a number of aspects related to the patient interaction with the vCare system which will need to be better taken into account. For now, the laboratory environment makes it easy for the patient, as every sensor and game is already installed and there is human support available at any time. The technical implementation is proving to be successful. We still need, however, to identify the barriers the patients will face in the home environment, when they will be in a position to entirely interact with the system by themselves. It is therefore important to reflect on all the complementary measures that need to be taken in order to provide the patient with a secure and trusted environment.
Positive developments
Patients are positive about the vCare system, and have shown an interest in, and readiness, to change in order to make use of vCare technology, including the vCoach avatar. They feel reassured knowing that will not be ‘left alone’ when they return home after their discharge from the hospital. They see the vCoach avatar as a truly supportive partner, and want to know how to interact with it. Patients understand that their future treatment will not be limited to taking pills. And realise that, in the absence of corrections to cardiovascular risk factors, the efforts of their medical team will not have been in vain.
Participatory Design tools and methods
When developing innovative healthcare technologies, acceptability and usability of the technology should be evaluated by users (i.e., medical staff and patients) throughout all the development phases, in order to guide the design process in accordance with user’s specific needs and reduce the risks of non-acceptance.
The methodological approach to drive the Participatory Design process has been derived from TUD experience[1] (Harst et al, 2020), which describes the methodology adopted for mapping different stages of a Participatory Design process during the development of IT healthcare applications.
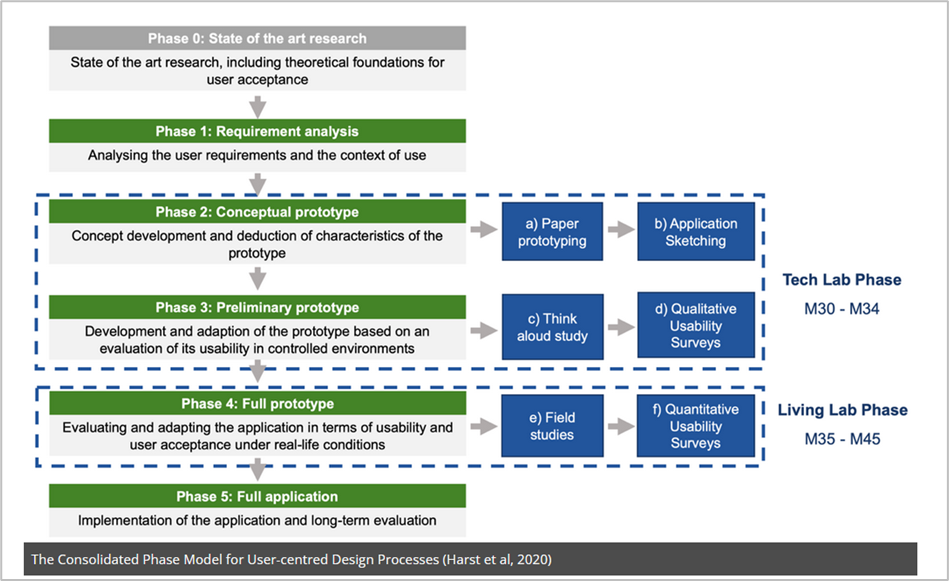
This is a 6 phases model where each phase features specific tasks and tools to gather user’s insights: Phase 0 (State of the art research), Phase 1 (Requirement analysis), Phase 2 (Conceptual prototype), Phase 3 (Preliminary prototype), Phase 4 (Full prototype), and Phase 5 (Full application).
In vCare, Phase 0 and Phase 1 have already been performed in previous phases, while the other phases have been mapped according to the time schedule of the upcoming tasks. Specifically, starting from the proposed methodology, we derived 6 stages for the Participatory Design approach: The Tech Lab includes the first 4 stages (Up to the preliminary prototype) while the last 2 ones are embedded in the Living Lab and Pilot Test activities.
To learn more on the clinical aspects of vCare platform please visit the project website
Please confirm you want to block this member.
You will no longer be able to:
Please allow a few minutes for this process to complete.